The art and science of exercise training and testing to help improve performance and health is for everyone.
The art and science of exercise training and testing to help improve performance and health is for everyone.
Summary
Monitoring the heart rate (HR) can help individuals personalize their aerobic exercise program and objectively measure progress. As a simple and practical measure of metabolic activity, intensity and stress, HR use is recommended and used by health practitioners, coaches, athletes in all sports, and others including beginners and those in rehabilitation. This paper outlines some of the health and fitness benefits of employing an appropriate individualized submaximal heart rate, called the MAF HR, determined by the 180 Formula, which corresponds to the physiological parameters of aerobic threshold (AerT) and maximal fat-burning (FATmax).
Introduction
Having researched and clinically employed HR monitoring professionally with a wide range of individual patients since the late 1970s, it became an integral part of the notion of maximum aerobic function (MAF), sometimes referred to as the Maffetone Method. As a biofeedback tool to help individuals exercise at a specific submax intensity, strict adherence to the MAF HR during an aerobic training period allowed them to develop increased speed, power and other fitness gains without exceeding the MAF HR, which also led to improved competitive performance. Various health benefits can also be realized during this process including better musculoskeletal support (muscle balance), increased fat-burning (FATmax) and glycogen-sparing, and prevention of overtraining (and related injuries).
Today, an accurate HR is easily obtained by simple technology that senses beats from the chest, wrist or ears. The full range of exercise HRs correspond to various physiological markers that reflect exercise intensity as it relates to physical, biochemical and mental-emotional stress. In particular:
- Physical activity at lower intensities emphasizes slow-twitch, red, aerobic muscle fiber development, while higher intensities emphasize fast-twitch, white, anaerobic fibers.
- Metabolic activity is associated with substrate utilization — the conversion of predominantly fat by aerobic muscle fibers and predominantly glucose by anaerobic fibers to produce energy (ATP) to power activity.
In the laboratory, a gas analyzer measures an individual’s oxygen and carbon dioxide to obtain substrate utilization as the respiratory exchange ratio (RER), also an indicator of relative activity levels. At lower exercise intensities, a larger percentage of energy is provided by free fatty acids and triglycerides, referred to here as fat. Higher intensities show the greatest amount of fuel is provided by glucose and its derivatives (stored glycogen, lactate, and blood glucose), referred to as sugar.
Increased fat-burning, especially at a maximal level (FATmax), is associated with improved health and better fitness. Properly trained athletes consuming a healthy diet are capable of burning significant amounts of fats throughout the range of increasing intensities, albeit lesser amounts at very high intensities — those with poor aerobic development are unable to do so. (Note that the consumption of refined carbohydrates can significantly reduce fat-burning even at lower exercise intensities.)
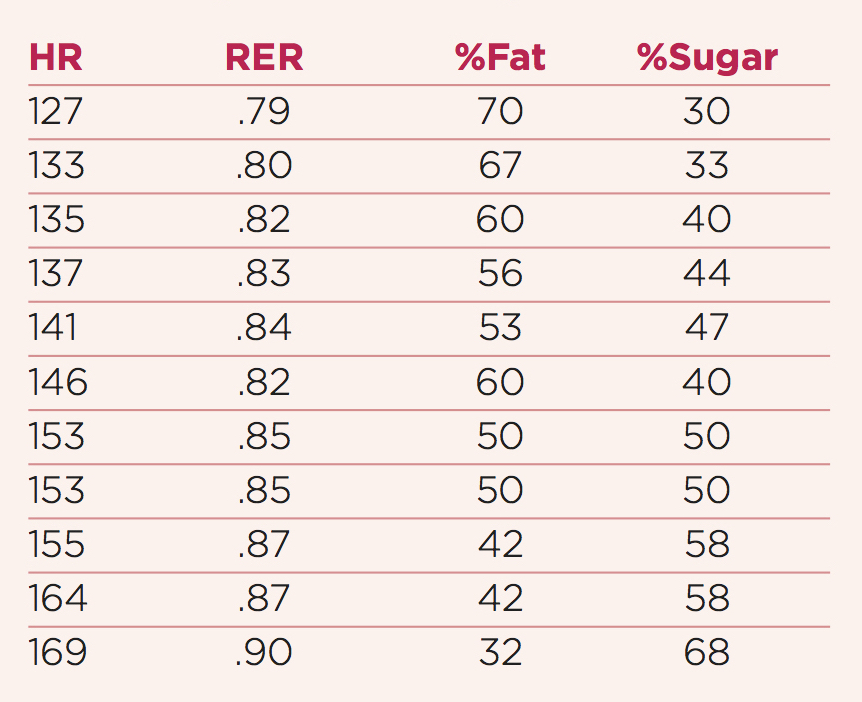
An example of the percentage of sugar and fat burned at increasing HR is shown in the table below.
Percentage of fat- and sugar-burning with related RER and heart rate (HR) in an aerobically fit and healthy athlete.
At 155 HR this athlete can run 5:25 per mile pace. Note the continued use of fat for energy, albeit lower, and impressive for a relatively high-intensity HR of 169.
Defining MAF HR
Critical changes in substrate utilization help define lower-intensity versus higher-intensity exercise:
Lower-intensity exercise occurs up to the point where the body’s use of fat for energy peaks — FATmax — after which sugar consumption quickly rises and fat lowers with higher-intensity exercise. Some authors also use FATmax as a threshold measure for exercise prescription, often referring to it as aerobic threshold (AerT).
As exercise HR and intensity are closely associated with substrate utilization and other metabolic activity (such as stress hormone and lactate production increasing with higher-intensity), the MAF HR is defined as the rate corresponding with AerT and FATmax. Training at this lower-intensity encourages:
- Maximum health benefits including cardiovascular, metabolic, immune, neuromuscular and brain function.
- Developing the aerobic system to increase work rate (running speed, cycling power, etc.) at the same MAF HR, and ultimately, improve competitive performance.
- Improved fat-burning, which can also help prevent or reduce excess body fat.
- Reduced incidence of injury.
- Prevention of moderate to high levels of post-exercise muscle fatigue and weakness.
- Increased ability to better recover from exercise of all intensities.
Studies show that the AerT is located at an exercise intensity that is often described as a percentage of maximum oxygen consumption or VO2max. This is sometimes referenced as 75 percent but it varies with and is largely determined by training and subsequent fitness, health status and age. For example, AerT occurs at a lower percentage for those who are untrained, ill, or elderly. Values may be higher for very well-trained elite athletes (such as an AerT of 80%+ of VO2max), and lower for untrained individuals (AerT as low as 55% of VO2max). The AerT occurs at a higher percentage for adolescents, and at a lower percentage for those over age 60. (These and other factors noted below, also apply in the determination of the MAF HR.)
Exercise Intensity
Exercise prescribed according to relative intensity is a mainstay in the scientific literature. It is intended to produce exercise stress that is approximately equivalent between individuals with different absolute exercise capacities. The traditional and common approach has often been to prescribe exercise intensity as a percentage of VO2max or maximum heart rate (HRmax).
However, exercise intensity prescribed at a percentage of these parameters does not necessarily place individuals at an equivalent intensity above resting levels. Some individuals will fall above or below metabolic thresholds of substrate utilization at the same percentage of VO2max or HRmax.
Furthermore, the most widely used estimation methods of exercise intensity by many individuals is to observe subjective parameters (such as the talk-test) or statistical observations about a population (such as heart-rate zones, the 220 Formula and others), which have no allowances for personalization. In the case of most exercising individuals, they do not accurately obtain VO2max, HRmax, RER or other physiological parameters with which to calculate an appropriate training intensity. This makes obtaining the MAF HR using the 180 Formula, discussed below, a practical and effective alternative.
In general, the two most commonly used exercise terms can be defined in relation to intensity and substrate utilization:
- Aerobic—lower-intensity activity with higher fat-burning (and glycogen-sparing) potential.
- Anaerobic—higher-intensity, lower fat-burning and higher sugar-burning (utilizing glycogen stores) potential.
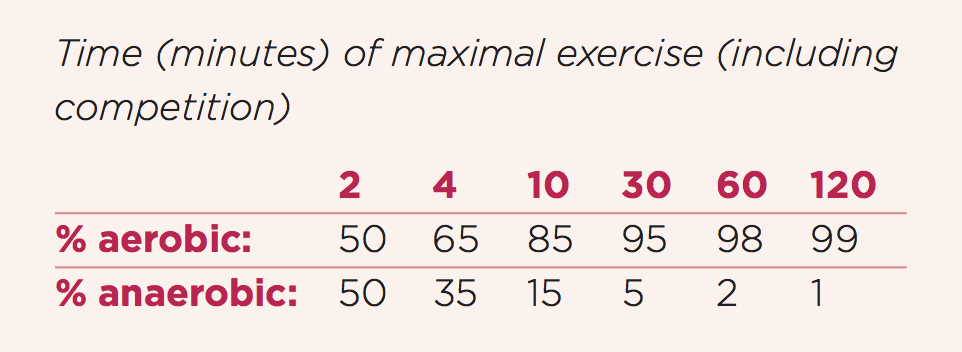
While the extensive aerobic and anaerobic systems work together, their separate functions are evident. This includes various physical and metabolic properties, such as muscle fibers and nerves, and hormonal, circulatory and immune factors. As systems, each has been long known to contribute proportionately to maximal exercise, including competition, with increasing aerobic contribution with increasing time, especially in endurance activities. This is highlighted in the table below.
Contribution of the aerobic and anaerobic systems during maximal physical exercise (adapted from Astrand PO and Rodahl K, and McArdle et al.).
Lower intensity
MAF emphasizes the importance that the majority of exercise over time should occur at a lower or submaximal intensity. This helps promote long-term health, manage stress and prevent injury, develop the aerobic system, improve fat-burning and improve endurance performance. Lower-intensity exercise also includes warming up, cooling down and easy training/recovery days. Modern humans are physiologically better adapted to exercise intensities similar to ones their hominid ancestors evolved with rather than those supported by modern societies (see Boullosa et al.). These would have included daily bouts of prolonged, low-intensity, aerobic-based activities, which are primarily fueled by the body’s long-term energy source: fat.
Lower-intensity exercise has also been described as regenerative by Meyer et al., since it activates and develops the organs, glands and other systems, and processes that together exhibit a series of interrelated functions that include:
- Endurance exercise capabilities.
- Protection from metabolic syndrome.
- Recovery from high-intensity activity.
- Resilience to oxidative stress (aging).
All these activities stem from the body’s ability to reliably and continuously draw from the aerobic system and its abundant fuel source (fats). This bolsters the metabolism and creates positive health outcomes due to its epigenetic effects on gene expression.
The diverse mechanisms implicated in these abilities include the respiratory and cardiovascular systems (lungs, heart and blood vessels), but most importantly the slow-twitch aerobic (Type I) muscle fibers, which also assist anaerobic (Type II) muscle fibers in their function during high-intensity efforts (see Haseler et al.). Training the aerobic system at levels associated with the MAF HR (and AerT and Fatmax), therefore, can contribute a wide range of health and fitness benefits to individuals in all sports.
Higher intensity
Exercise at higher intensities is associated with the increased use of sugar, which is much more limited in supply than fats. Using sugar for energy allows the body to increase its energy production and work rate far beyond what the rate of oxygen uptake and aerobic metabolism allows. (When the rate of sugar usage exceeds the supply of oxygen, this sugar is burned anaerobically, or outside the presence of oxygen.)
Anaerobic, high-intensity exercise raises the risk for:
- Higher levels of physical and biochemical stress.
- Reduced immune function.
- Slower muscular repair/longer recovery.
- Increased inflammation.
- Increased risk of muscle injury (most common in fast-twitch fibers).
- Reduced or impaired fat-burning.
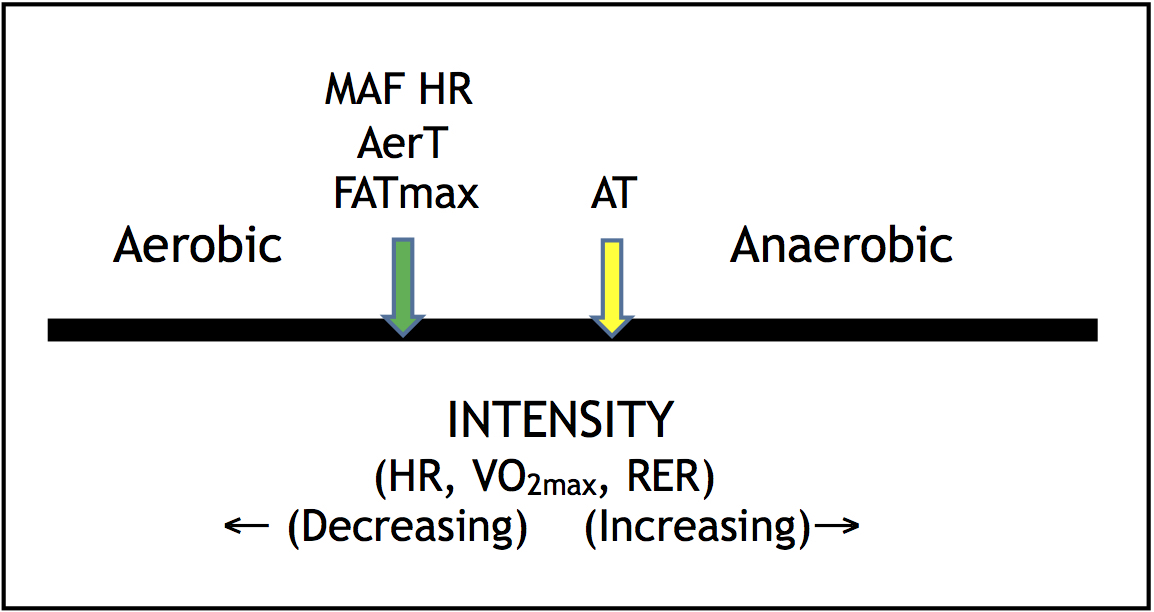
High-intensity exercise requires a significantly longer time for recovery (typically two to three days versus one day for a lower-intensity aerobic workout), and is a common component of and contributor to the overtraining syndrome. In addition to anaerobic activity associated with reduced fat-burning, it also marks the rise of lactate, a point called the anaerobic threshold (AT), indicative of the start of glycogen depletion, as shown in the figure below.
While high-intensity training can be a positive stress that promotes various fitness benefits, including competition, a well-developed aerobic system should precede its development.
The general relationships between MAF HR, AerT, Fatmax, and AT; aerobic and anaerobic; heart rate, VO2max and RER; and intensity.
Calculating MAF HR: The 180 Formula
A method developed in the early 1980s to determine one’s MAF HR, without laboratory or other evaluations, is the 180 Formula. Based on feedback from others who employ laboratory measures, comparisons to the MAF HR are similar.
I derived the 180 Formula after a few years of determining the MAF HR in large numbers of individuals via an array of clinical assessments, including age, a comprehensive physical evaluation, gait analysis at wide ranges of HRs, health and fitness history; and in some cases, with confirmation using measures of gas exchange. Initially, it became clear that a HR equivalent to 180 minus age could constitute the beginnings of a potential formula for determining a person’s MAF HR, with additional modifications developed soon afterwards. (Only after this period would the relationships between MAF HR, AerT and Fatmax be realized.)
The 180 Formula indicates that, following the subtraction of one’s age from 180 (a number that is only a means to an end), certain important modifications must be made depending on a person’s health and fitness status. These factors further influence the final MAF HR, and are key aspects of individualization. Below is the most up-to-date (2019) 180 Formula.
The 180 Formula for determining the MAF HR
Subtract your age from 180, then modify from one of the categories below:
- If you have or are recovering from a major illness (heart disease, any operation or hospital stay, etc.), are in rehabilitation, are on any regular medication, or are in Stage 3 (chronic) overtraining (burnout), subtract an additional 10.
- If you are injured, have regressed or not improved in training (such as poor MAF Tests) or competition, get more than two colds, flu or other infections per year, have seasonal allergies or asthma, are overfat, are in Stage 1 or 2 of overtraining, or if you have been inconsistent, just starting, or just getting back into training, subtract an additional 5.
- If you have been training consistently (at least four times weekly) for up to two years without any of the problems mentioned in a) or b), no modification is necessary (use 180 minus age as your MAF HR).
- If you have been training for more than two years without any of the problems listed above, have made progress in your MAF Tests, improved competitively and are without injury, add 5.
Exemptions:
The 180 Formula may need to be further individualized for athletes over the age of 65. For some, up to 10 beats may have to be added for those only in category (d) of the Formula. This does not mean 10 should automatically be added, but that an honest self-assessment be made.
For athletes 16 years of age and under, the formula is not applicable; rather, an MAF HR of 165 has been used.
The 180 Formula is not a replacement for properly executed laboratory testing that determines the AerT, Fatmax and other metrics, although it usually corresponds well with them. Given that the 180 Formula is simple and applicable to a majority of the population, the MAF HR can help individuals monitor workouts, improve submax fitness and competitive performance, prevent overtraining, and build health. This makes it very useful to those who do not have access to regular laboratory testing.
Assessing Submax Aerobic Speed
Developing the aerobic system while training at the MAF HR should result in increasing speed and/or power, and can be an important physiological forecast of endurance race performance. Studies show that submax thresholds are the best predictors of endurance performance in runners, cyclists, race walkers and other athletes, as well as in the general performance of untrained people. Increasing speed or power at the same submax HR translates to improved aerobic function, including fat-burning, and can predict faster race performances.
Heart rate assessment of submax activity can accurately inform athletes, coaches and clinicians on training status, especially with improvements in AerT, Fatmax and MAF HR. These are sometimes observed relatively quickly (such as within a week or two after the start of an endurance training program). If improved performance at MAF HR does not occur within a month or two, consider lowering the MAF HR (or re-evaluate the 180 Formula), and assess other lifestyle stress (especially diet, since refined carbohydrates can impair fat-burning and the aerobic system).
While improved speed or power typically reflects a state of functional overreaching, the onset of overtraining (nonfunctional overreaching) can be indicated by reduced AerT and FATmax, with performance progress at the MAF HR plateauing or declining following a period of progress.
By training at the MAF HR, and building the aerobic system, improvements are expected as indicated by increased performance at the same MAF HR — even without high-intensity training. This maximum aerobic function, MAF, can be tested various ways by comparing HR and some metric such as run pace or cycling power.
The MAF Test
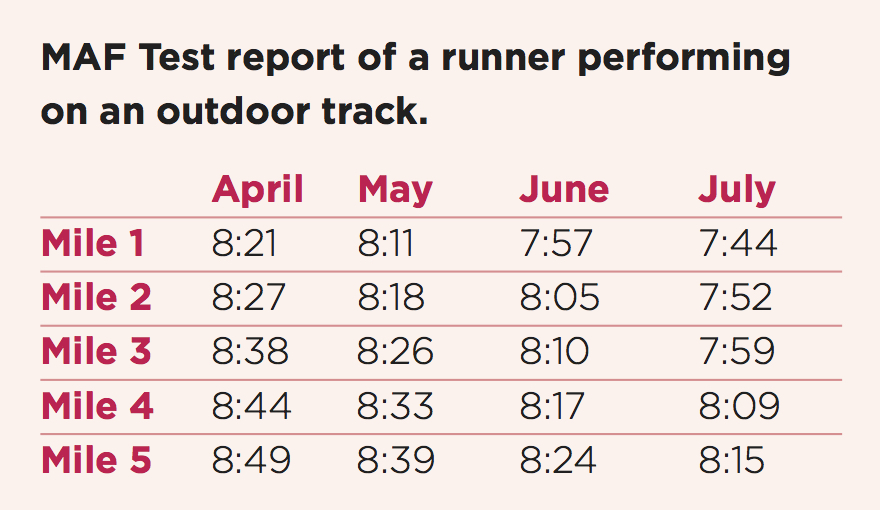
Developed for everyone who exercises, especially for use by competitive athletes, coaches and clinicians, the MAF Test tracks changes in submax pace, speed, power, or other metrics, which reflects the improvement of the aerobic system across time. For a runner, this test may consist of a 3- to 5-mile run on an oval, 400m track, while recording the time per mile (or kilometer), as seen in the table below. (A walker, beginning exercisers or one in rehabilitation can use a shorter distance, such as one mile.) It can also be performed with a GPS heart monitor on a road or trail, with other activities also used for the MAF Test, including cycling and rowing by measuring power, swimming by measuring laps, walking pace, etc.
The MAF Test should be preceded by a 15-minute easier warm-up and performed under consistent conditions (similar shoes, weather, time of day, location, etc.). The table below shows the results of a runner’s MAF Test over a four-month period.
Certain lifestyle factors can impair the aerobic system, leading to reductions in speed or power at the same MAF HR (along with resting HR). These include excess exercise volume and/or intensity, mental-emotional stress, irregular gait, or others that increase sympathetic activity and raise HR. The diet also can play a primary role, with the intake of refined carbohydrates reducing aerobic development through neuroendocrine stress.
Conclusion
Determining the MAF HR by the 180 Formula is a useful method for obtaining an effective submax training HR that does not require laboratory or other testing. This personalized approach can be used for effective training, monitoring progress, and also can lead to improved competitive performance and health while preventing overtraining.
Bibliography
Achten J, et al. Determination of the exercise intensity that elicits maximal fat oxidation. Med Sci Sports Exerc. 2002; 34: 92-97.
Astrand PO, Rodahl K. Textbook of Work Physiology. New York, McGraw-Hill 1977.
Bassett DR, Howley ET. Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med Sci Sports Exerc. 2000;32(1):70-84.
Billat V, et al. The Concept of Maximal Lactate Steady State. Sports Med. 2003;33(6):407-426.
Blankenbaker DG, De Smet AA. MR imaging of muscle injuries. Appl Radiol. 2004:14–6.
Boullosa D, et al. Do Olympic Athletes Train as in the Paleolithic Era? Sports Med. 2013;43(10):909-917.
Boyd A, et al. Lactate inhibition of lipolysis in exercising man. Metabolism. 1974;23(6):531-542.
Buchheit M. Monitoring training status with HR measures: do all roads lead to Rome? Front. Physiol., 27 February 2014.
Buchheit M, et al. Monitoring endurance running performance using cardiac parasympathetic function. Eur. J. Appl. Physiol. 2010;108:1153–1167.
Cipryan L, et al. Effects of a 4-Week Very Low-Carbohydrate Diet on High-Intensity Interval Training Responses. J Sports Sci Med. 2018;17(2):259-268.
Dantas JL, Doria C. Detection of the Lactate Threshold in Runners: What is the Ideal Speed to Start an Incremental Test? J Hum Kinet. 2015;45(1):217-24.
Decroix L, et al. Can the Lamberts Submaximal Cycle Test Reflect Overreaching in Professional Cyclists? Int J Sports Physiol Perform. 2018;13(1):23-28.
Ellis AC, et al. Respiratory quotient predicts fat mass gain in premenopausal women. Obesity. 2010; 18(12): 2255-2259.
Emerenziani GP, et al. Effects of Aerobic Exercise Based upon Heart Rate at Aerobic Threshold in Obese Elderly Subjects with Type 2 Diabetes. Int J Endocrinol. 2015;2015:695297.
Haseler LJ, et al. Skeletal muscle phosphocreatine recovery in exercise-trained humans is dependent on O2 availability. J Appl Physiol. 1999; 86:2013-8.
Hickson RC, et al. Effects of increased plasma fatty acids on glycogen utilization and endurance. J Appl Physiol. 1977; 43: 829-833.
Høeg T, Maffetone P. The Development and Initial Assessment of a Novel Heart Rate Training Formula. Poster presented at the Medicine & Science in Ultra-Endurance Sports 2nd Annual Conference; May 2015; Olympic Valley, CA, USA.
Holloszy JO, Coyle EF. Adaptations of skeletal muscle to endurance exercise and their metabolic consequences. J Appl Physiol. 1984; 56: 831-838.
Kindermann W, et al. The significance of the aerobic-anaerobic transition for the determination of work load intensities during endurance training. Eur J Appl Physiol. 1979;42(1):25-34.
Kreher JB, Schwartz JB. Overtraining Syndrome. A Practical Guide. Sports Health. 2012; 4(2): 128–138.
Londeree BR. Effect of training on lactate/ventilatory thresholds: a meta-analysis. Med Sci Sports Exerc. 1997;29(6):837-843.
Maffetone P. Complementary Sports Medicine. Champaign, IL: Hum Kinet; 1999.
Maffetone P. White Paper. An Introduction to MAF: Maximum Aerobic Function. Independent; 2016.
Maffetone PB, Laursen PB. Athletes: Fit but Unhealthy. Sports Med Open. 2015;2:24. Epub 2016 May 26.
Malhotra A, et al. It is time to bust the myth of physical inactivity and obesity: you cannot outrun a bad diet. Br J Sports Med. 2015;49(15):967-8.
Mann T, et al. Methods of prescribing relative exercise intensity: physiological and practical considerations. Sports Med. 2013;43(7):613-25.
Mattson M, et al. Meal frequency and timing in health and disease. Proc Natl Acad Sci. 2014; 111(47): 16647-16653.
McArdle W, et al. Exercise Physiology. 3rd ed. Philadelphia, PA: Lea & Febiger; 1991.
Meyer T, et al. A Conceptual Framework for Performance Diagnosis and Training Prescription from Submaximal Gas Exchange Parameters: Theory and Application. Int J Sports Med. 2005;26:S38-S48.
Montgomery P, et al. Validation of Heart Rate Monitor-Based Predictions of Oxygen Uptake and Energy Expenditure. J Strength Cond Res. 2009;23(5):1489-1495.
Powers SK, Jackson MJ. Exercise-Induced Oxidative Stress: Cellular Mechanisms and Impact on Muscle Force Production. 2008. Physiol Rev. 2008;88(4): 1243-1276.
Putman CT, et al. Effects of short-term submaximal training in humans on muscle metabolism in exercise. Am J Physiol. 1998;275:E132–E139.
Schutz Y. Abnormalities of fuel utilization as predisposing to the development of obesity in humans. Obesity Res. 1995; 3(2): 173s-178s.
Siegl A, et al. Submaximal Markers of Fatigue and Overreaching; Implications for Monitoring Athletes. Int J Sports Med. 2017;38(9):675-682.
Szivak T, et al. Adrenal Cortical Responses to High-Intensity, Short Rest, Resistance Exercise in Men and Women. J Strength Cond Res. 2013;27(3):748-760.
van de Vyver M, et al. Neutrophil and monocyte responses to downhill running: Intracellular contents of MPO, IL-6, IL-10, pstat3, and SOCS3. Scand J Med Sci Sports. 2015; 26(6):638-47
Volek J, et al. Rethinking fat as a fuel for endurance exercise, Eur J Sport Sci. 2015; 15:1, 13-20.
Walsh N, et al. Position statement part one: immune function and exercise. Immunol Rev. 2011;17:6-63.
Yoshida T, et al. Blood lactate parameters related to aerobic capacity and endurance performance. Eur J Appl Physiol Occup Physiol. 1987;56:7–11.