This very common and debilitating health problem is now so prevalent worldwide that preventing it has almost been abandoned; instead of finding the cause, controlling pain has become the default treatment of choice.
At one time, back pain — anywhere along the spine, including the neck — was usually not much more than an annoyance. “Take two aspirin and call me in the morning” was the most common recommendation. Along the way, “low” back pain grabbed all the headlines as it may be the most vulnerable area to stress and strain, wear and tear; but muscles and joints in other spinal areas can cause just as much pain.
Today, things have not really changed much, although the meds are often prescribed for daily use, and are much stronger and more addictive. This disability also appears more disabling and disturbing — and its incidence has skyrocketed worldwide.
A recent study in The Lancet showed what we already knew — that low-back pain is an exploding and serious global problem not being addressed well in healthcare overall, and mainstream medicine in particular. And that scientists have not found “the cause” or even much about the problem other than to claim “more research is needed.” Of course, the causes are often multiple, individual and don’t usually show up on an X-ray or blood test. Even pain is elusive; a difficult emotion to measure.
The result is that many back pain patients continue to suffer, with new cases coming on board daily, including the most unlikely victims: children. (No surprise as children now develop “adult” conditions like Type 2 diabetes and nonalcoholic liver disease.)
I’ve spent my career helping patients with back pain by finding the causes using thorough personalized assessments (the most important part of the process) and treatment (a combination of lifestyle changes and biofeedback). I also have the very valuable experience of learning about the condition from my own serious struggle with low-back pain, now long gone.
In most cases of back pain, the body fixes its own problems. This happens best and faster in a healthier more fit body and is the most important starting point. This can also prevent the problem in the first place.
The key is the cause
In most cases of back pain, the cause is not often immediately apparent to the patient or practitioner. While it’s important to first rule out such rare but serious causes as malignant disease, spinal fracture or true malformation, it’s not unusual to be left with relatively minor problems as the primary cause. In addition, despite the location of pain, the back itself is usually not the cause.
Without knowing the cause, therapy is often unsuccessful, unless the body corrects itself and the problem resolves (not an uncommon outcome).
Three common causes of low back pain include:
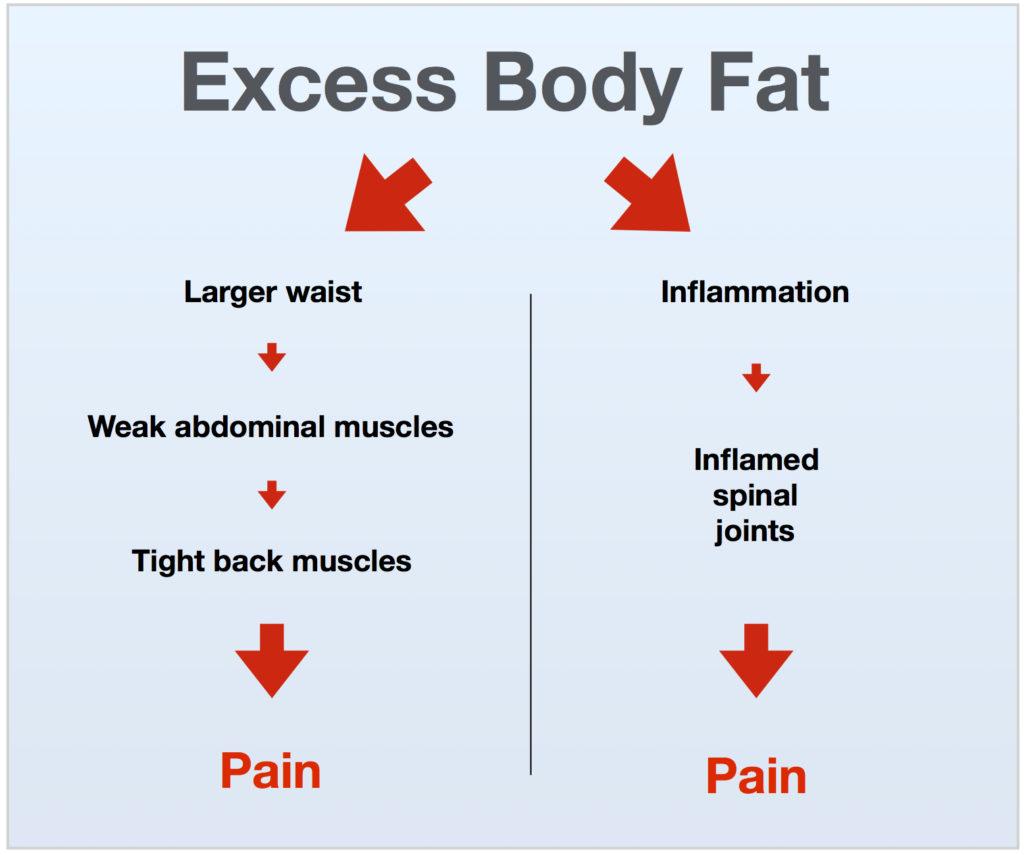
- A larger waist, from excess body fat, triggering weak abdominal and tight back muscles, and pain.
- Chronic inflammation, due to the combined excess body fat and poor diet, triggering pain in spinal joints.
- Muscle imbalance, which puts physical stress on spinal joints producing inflammation and pain.
These conditions often occur together, forming a vicious cycle of chronic back pain. Other lifestyle factors can worsen the condition:
- Too much sitting.
- Being sedentary.
- Exercise stress.
- Bad shoes.
- Poor sleep.
Unfortunately, symptom treatment is the most common approach to low back pain. This usually means the cause is not found or eliminated, and the problem recurs, becoming a chronic disability.
Meanwhile, therapeutic success has been found most through approaches other than mainstream medicine. These include hands-on assessment and treatment of muscle imbalance through biofeedback, including physical therapy, kinesiology, spinal manipulation, and massage therapy. Lifestyle remedies that reduce body fat and chronic inflammation must be part of this process.
Unfortunately, not all back pain patients are referred or recommended to these practitioners by primary care doctors, despite the success and scientific basis of the approaches.
Remedies out of the so-called mainstream are suspect in great part because there are so many ineffective and quack-like treatments, pills, and devices/braces that continue to flood the market — it seems there’s always a new gadget or supplement that supposedly cures back pain when in fact they almost never work.
The idea of complementary medicine — which combines the best of alternative with mainstream approaches — is ideal for back pain patients, but utilized less often. This may involve referrals back and forth between more than one practitioner, something done too infrequently. Today’s standard of care, unfortunately, regardless of the type of practitioner, is to cut short the time-consuming evaluation process, and apply some predetermined treatment. For practitioners using only one therapeutic tool such as massage, manipulation, acupuncture, or nutrition, all of which may have great value, if a patient requires two or more types of care, applying just one may not work as well — another point where referrals are important but often not made.
In our current healthcare mode of ‘this remedy for that symptom,’ there’s almost no place for conditions with more than one cause, and therefore more than one specific treatment. For example, a large waist is a common problem in people with low back pain, in part because the abdominal muscles are weak, causing the back muscles to tighten. Strengthening the abdominal muscles appears to make sense. But attempting this through exercise can make the problem worse by adding more physical stress to the low back long before any strength benefits are realized.
In this example, a more effective and faster remedy would be to:
- Address muscle imbalance through hands-on care.
- Address inflammation by eliminating dietary sugar and other refined carbohydrates , and unhealthy fats.
- Make other necessary lifestyle changes (associated with sitting, bad shoes, excess stress, and sleep).
In many cases, low back pain is a self-limiting condition, meaning the problem disappears on its own (the body is always trying to correct itself). This is commonly seen in those with a minor, and sometimes severe, back pain that goes away in a few days. However, as mentioned above, a healthier body can accomplish this much better.
A common blame for low back pain is the lack of exercise. Certainly being sedentary can contribute to back pain, while being physically fit and healthy can prevent it. But performing exercise as a therapy when in pain, especially in the presence of muscle imbalance and inflammation, for example, can often aggravate back pain. In fact, many people develop or worsen back pain due to some aspect of their exercise program, such as overtraining, or stretching.
An inactive lifestyle is more often the cause — even those who exercise are sometimes inactive for most of the day. Part of the problem is our increased sitting time, a position stressful for the whole spine. Eating, driving, working, and the perception of relaxing are usually associated with sitting stress.
Stress is another common blame for back pain. No doubt some form or combination of physical, biochemical or mental-emotional stress plays the major role in the problem, like those noted above. But telling a patient their problem is due to stress — like aging — is a healthcare injustice. Likewise, for the term “slipped disc,” sometimes referred to a ruptured disc. For every patient with low back pain and X-ray indicating a disc problem, there are a hundred other patients with the same X-ray findings who don’t have pain. And, even with successful therapy, X-ray findings don’t usually change.
Anatomy of low-back pain
The fact that low back pain has risen more than 50 percent worldwide since 1990 demonstrates that it has paralleled the global overfat pandemic.
This is because back pain is often associated with excess body fat, particularly belly fat, leading to tight low-back muscles. This condition is prevalent in those with carbohydrate intolerance, and goes hand-in-hand with chronic inflammation. This can affect spinal joints, so even if you get the right hands-on treatment, the problem can come back when these two primary conditions are not addressed.
When Back Pain Comes Back
As eluded to above, when back pain comes back it usually means the cause of the problem has not been properly addressed.
Various treatments can help temporarily, but the problem returns. This, of course, is due to addressing the symptoms and not the cause. (In addition, the placebo effect from home remedies and from therapists is powerful, and real.)
The most effective treatments begin with a proper assessment that determines the cause of the problem, not an off-the-shelf remedy.
Suggestions for dealing with back pain:
- Avoid using heat on inflamed areas; use cold, but avoid ice directly on the skin.
- Rule out serious conditions (usually by your primary care or other practitioner).
- Avoid grabbing for more extreme treatments first unless it is clearly warranted. For example, rather than surgery first, seek conservative care.
- Ask friends or relatives about their success with certain practitioners, especially those who are holistic, healthy and fit.
- The more successful therapist spends a good amount of time evaluating before treating.
- If your back pain is not better after a few hands-on treatments, that approach may not be best/working for you — avoid the notion that it took many months to develop your problem and could take the same time to correct it.
Back pain is big business
Anti-inflammatories and pain killers may mask the problem, but will not fix it, and come with their own set of problems. Pain control is, by virtue of the name, symptom treatment, not a cure. We don’t want to control pain, we want to eliminate its cause, which obviously will get rid of the pain too.
Practitioners who know too little about low back pain should not be allowed to treat it by just prescribing medication to control pain. Likewise, the idea of “learning to deal with pain” is unacceptable too. These are key causes of the opioid-addiction epidemic.
Using a holistic approach is important too. Even the right remedy can cause back pain to return. For example, a successful hands-on remedy that is just what the patient needs can be negated while walking out of the clinic in bad shoes, such as those with thicker or higher heels commonly worn by many people.