How the human population can develop its own natural defense to COVID-19
Herd immunity for COVID-19 has probably been building for several months since the virus was first detected in China. However, the lingering question remains: How will this pandemic play out? This question is even more important when you consider that an effective vaccine appears to be well in the future.
Beginning with our earliest ancestors, humans have successfully developed protection against infections through a healthy immune system. This includes a complex antibody mechanism that fights invading viruses, bacteria and other organisms. It evens remembers most of them in case they return. White blood cells, bone marrow, the spleen and other systems within the body are enlisted in the process. In fact, most of our body plays some part in immunity, including the skin, tears, saliva, stomach and especially the brain.
Natural immunity can also be boosted by certain vital nutrients found only in healthy foods. In addition, vitamin D is another requirement for healthy immunity, and is best acquired from safe sun exposure.
Conversely, unhealthy foods can impair immunity for at least two main reasons:
- Junk food replaces nutrient-rich healthy food.
- Refined carbohydrates (almost all those consumed), including sugar, quickly lead to excess body fat, promoting chronic inflammation and disease significantly raising the risk of infection.
Mental and emotional stress can also impair immunity, including when panic ensues from media hype and false rumors about infections (a form of herd mentality).
Natural Immunity
Our immune systems are always exposed to viruses and other pathogens. In a healthy body, this can trigger the production of antibodies against the organisms, which usually prevents illness or minimizes the infection, and often leads to natural lifelong active immunity against that virus. During an outbreak or a pandemic, as increasing numbers of individuals develop natural immunity, a population-wide effect called herd (or community) immunity can occur, reducing the risk and spread of infection.
It appears that about 50 percent of a population requires exposure to a virus, bacteria or other pathogen for natural herd immunity to develop (some experts think COVID-19 may be higher, but we don’t know yet). Natural immunity is indicated by the presence of antibodies against the particular pathogen, as evaluated by a blood test.
Meddling with Mother Nature
Natural immunity is often impaired in those with heart disease, pulmonary disease, diabetes and other chronic illness, significantly raising the risk for COVID-19 and other infections. Excess body fat can cause all these conditions, and directly impair immunity.
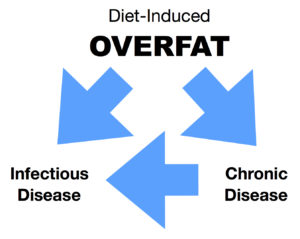
The graphic below demonstrates the relationship between overfat increasing the risk of both chronic disease and infection, while chronic disease itself also increases the risk of infection. Moreover, overfat is usually diet-induced, primarily from consumption of sugar and other refined carbohydrates.
Overfat can also increase viral shedding, increasing the spread of infection, and raise the risk of complications during an infection, including increased mortality. As 80 percent or more of the world is overfat, it’s no surprise that despite modern healthcare and public health efforts we are still vulnerable to infectious pandemics.
Artificial Immunity
Modern medicine has created a wide variety of vaccines. Just like overfat can impair natural immunity, it can also render artificial immunity from vaccines less effective.
Based on the concepts of herd immunity, indirect protection can also occur with a vaccine. Even those without natural or artificial immunity other individuals can still be protected from infection by virtue of those who get vaccinated. So vaccinating 100 percent of a population to reduce infection rates or end a pandemic may be unnecessary. For example, vaccinating 80 percent of only high risk individuals could protect most of the population as this may achieve a herd immunity threshold.
Even childhood infections such as measles, mumps, rubella, pertussis, chickenpox, and polio may be checked without everyone being immune — maintaining a certain threshold of immune individuals appears relatively successful as illness is maintained at what experts call “tolerable” levels.
What remains most important is to target overfat, poor diet and resulting ill health as the direct and indirect causes of poor immunity. This is also the most sensible public health action — one yet to be implemented.
While young children have yet to develop full natural immunity, they may still have reduced risk depending on the pathogens (such as with COVID-19). And many elderly people have impaired immunity — not because of age but due to chronic overfat and downstream chronic disease. Older individuals following healthy lifestyles, especially great eating habits, could still have healthy immune systems.
Unfortunately, a large part of the population is reactive, waiting for an illness to strike, or the threat of one, before actively working to improve their health. But good health is contagious, and as each of us proactively pursues it we also can help others.
Related links
References
Fine P, et al. “Herd Immunity”: A Rough Guide. Clin Infect Dis. 2011;52(7). doi: 10.1093/cid/cir007.
Maffetone P, Laursen P. The Perfect Storm: Coronavirus (COVID-19) Pandemic Meets Overfat Pandemic. Front. Public Health. 2020;8:135. doi: 10.3389/fpubh.2020.00135.
Metcalf CJE, et al. Understanding Herd Immunity. Trends Immunol. 2015;36(12). doi: 10.1016/j.it.2015.10.004.
Park HL, et al. Obesity-induced chronic inflammation is associated with the reduced efficacy of influenza vaccine. Hum Vaccin Immunother. 2014;10. doi: 10.4161/hv.28332.