
The white stuff may be the most common and primary addiction — a cycle that starts with a stressed brain, triggering further unhealthy eating. Breaking this vicious cycle starts with understanding it.
Sugar addiction is universally rampant and a leading cause of ill health and disease. Few people, however, realize that addiction to this dangerous substance is also at the root of other addictions as well — including alcohol, legal and illegal drugs, and even vices such as gambling, sex, shopping and working too much.
Most people with addiction issues tend to believe their personal compulsion or obsession is the worst of the world’s addictions. The fact is an addictive personality housed in the brain plays a primary role in the addictive process.
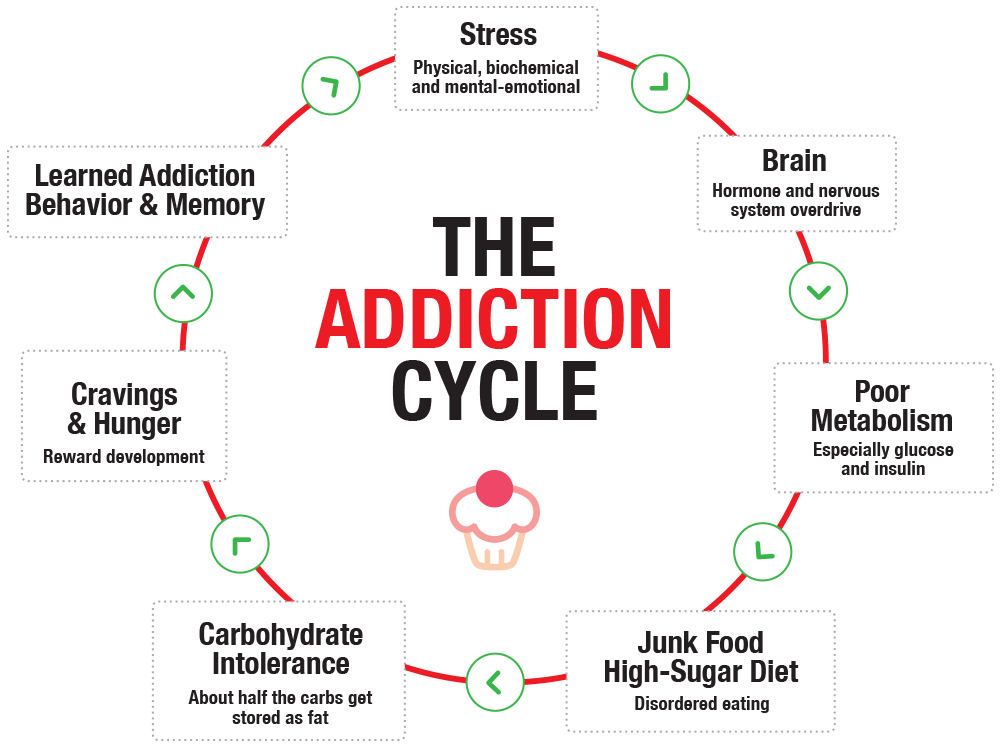
Feeding the brain with artificial rewards is a primary problem that must be addressed if addiction is to be properly remedied. The brain is influenced by lifestyle, which influences actions. In the case of addiction, this means seeking unhealthy habits that reward the brain. The highly complex process goes something like this:
- Physical, biochemical and mental-emotional stress affects the brain.
- These stresses affect the body’s metabolism in an unhealthy way.
- Stress leads to carbohydrate cravings.
- Cravings can lead to disordered eating.
- The use of drugs or actions that reward the stressed brain follows.
- This leads to what is known as addiction.
- As poor diet further impairs the metabolism, it usually increases body fat. (Those who don’t end up with increased body fat still have the metabolism of an overfat person.)
- And the cycle continues . . .
Since the immediate and long-term influence of carbohydrate food can dramatically impact the brain, influencing the metabolism and cravings, stress and poor dietary habits are the two main factors that fuel the addiction cycle.
Lifestyle Stressors
Drs. Rajita Sinha and Ania Jastreboff from Yale University School of Medicine have extensively reviewed the published research on this topic in “Stress as a common risk factor for obesity and addiction” in the journal Biological Psychiatry (May 2013), and the topic is also researched by other experts in this field.
My perspective is as a clinician, with many years of helping people eliminate the causes of addictions. Stress is almost always a key factor. It comes in many forms and often plays a key role in instigating the addiction cycle:
- Physical stress such as muscle and joint problems, dental neglect, neck pain, foot problems, excess sitting, poor posture or gait.
- Biochemical stress including hormone imbalance, digestive problems, poor diet and drug problems (excess alcohol or caffeine, nicotine, cocaine, etc.), prescription and over-the-counter drugs.
- Mental-emotional stress can be seen in poor personal relationships with people both personally and professionally. This may be partially due to physical pain, brain injury, confusion or lack of understanding about one’s health, such as how best to eat or work out, and even understanding addiction.
The accumulation of stress adversely affects the brain, impairing metabolism, and causing abnormal blood sugar and insulin levels, leading to carbohydrate cravings. One common reward-seeking behavior is eating refined carbohydrates, AKA sugar. Eating these foods affects the brain’s reward center. Addiction follows, and if one does not address this key factor, the vicious cycle continues.
The process also leads to increased body fat, weight and BMI, adding to more disordered eating, and more stress. While some people reduce food intake as a result of stress, many people eat more, especially through added snacking on junk food.
Addressing addictions by removing secondary substances such as alcohol, nicotine or cocaine, while a positive step in the process, may not break the addiction cycle because the primary problems in the brain and metabolism that influence cravings and the need for rewards remain. Often, the person finds another addictive substance, or just continues rewarding the brain with sugar, maintaining addiction.
Let’s look at the addiction mechanism with a wider more detailed view.
Brain Overdrive
Mechanisms in the hormonal and nervous systems are responsible for the brain’s stress response. While this mechanism is intended to help us adapt, the ongoing driving stress can lead to disordered eating and addictive behavior, along with reduced immune function, chronic inflammation, impairment of glucose metabolism, and carbohydrate intolerance. Some end-result signs and symptoms include:
- Increased body fat.
- Weight gain.
- Fatigue.
- Physical injury.
- Pain.
- Intestinal dysfunction.
- Infections and other illness (e.g., allergies and asthma).
- Increased hunger.
- Cravings for sweets.
- Poor sleep.
- Hormone imbalance.
- Metabolic syndrome.
- Overtraining syndrome (in people who exercise).
When chronic, the process of disease development follows:
- Diabetes.
- Alzheimer’s.
- Cancer.
- Cardiovascular disease.
- Associated conditions such as high blood pressure, stroke, high blood cholesterol and triglycerides, cognitive dysfunction such as memory loss, and poor quality of life.
Reward: Food
Food reward is a behavioral issue common with stress, with sugar singled out as the most common food. Continuing to consume it can maintain the vicious cycle with stress triggering a desire for a sweet reward, followed by addiction and more food stress.
Basically, as researcher’s Sinha and Jastreboff write, stress potentiates cravings for desserts and other carbohydrates. Stress also diminishes emotional, visceral and behavioral control, while increasing impulsivity and leading to greater use of reward.
In addition, it does not take long for the brain to learn the reward, with memory and emotional processes involved in negotiating behavioral and cognitive responses.
Sweet foods are rewarding, stimulating the brain’s reward pathways and, via learning and conditioning mechanisms, increasing the likelihood of seeking out more sugar, just like the incentive that draws people to drugs like alcohol, nicotine and cocaine. Studies show that those with higher body fat seek rewards more easily.
The clinical indications of these addiction patterns were evident many years ago, and the most effective approach in dealing with addiction for my patients — and me — was simple: Eliminate the sugar addiction first, then any and all other addictions to drugs or other issues would more easily be eliminated.
The Fix: Break the Sugar Addiction Cycle
It was not long ago that the mention of sugar addiction would be countered by questions such as, “what?” or, “where’s the research?”
Today, many clinicians, researchers and most others have jumped on the sugar addiction bandwagon with a new common question: “How do I know when my sugar addiction is gone?” Like other addictions, the short answer is simple: when sugar no longer controls you. More importantly, when addiction itself no longer controls you.
Others ways we know include:
- When the sugar devil no longer can tempt you.
- When you stop rationalizing that refined carbs are part of a healthy diet.
- When you no longer believe that humans are glucose-dependent.
- When you understand that sugar does not give you long-lasting healthy energy.
After reviewing some of the mechanisms behind the very common problem of sugar and other secondary addictions, here’s the key point: The remedy is simple — breaking the cycle. I don’t wish to oversimplify an emotionally painful and complex physiological condition, but this involves reducing stress, especially from the diet. While individuality is important, in my experience there are two starting points:
The Stress List. This can help you organize your primary physical, biochemical and mental-emotional stresses in a way that begins the process of eliminating some, reducing others, and helping the body best adapt to those that remain.
The Two Week Test. This helps break the stress cycle by reducing excess carbohydrate foods, addressing sugar addiction, and helping to learn intuitively how to individualize healthy eating habits.








