A three-stage spectrum disorder defined
Summary
Overtraining has been traditionally described as diminished athletic performance that results from excessively increased training volume and/or intensity and competition. But the bigger picture is often elusive as the problem can be complex, necessitating a holistic view. Overtraining refers to an imbalance of, or maladaptation to, physical, biochemical and/or mental-emotional stress in an athlete’s life. While it can be deceptive and develop almost without warning, overtraining can affect health while impairing any aspect of human performance, including enjoyment of sport.
While the basic concept of overtraining as an imbalance appears simple, its complexity and lack of a single-test diagnosis can also contribute to the lack of consensus among athletes, coaches, health practitioners, and scientists on its definition. This despite extensive research on the topic of physical, biochemical and mental-emotional stress that is nearly a century old. The result is that this common and serious disorder can go untreated, especially in the early stages, and makes preventing it appear even more difficult.
This paper defines the overtraining syndrome as a three-stage spectrum disorder, following the stress model first described by Hans Selye (who also coined the term stress) in the 1930s. Its signs and symptoms are highlighted, with training, dietary and other lifestyle recommendations to help prevent and treat the condition.
Introduction
Overtraining (OT) occurs in all sports, from track and field to endurance, football and baseball, golf and tennis, and even in those who exercise regularly but don’t compete. (The term overtraining is best reserved for individuals engaged in exercise, whereas a nearly identical condition, burnout, refers to parents, teachers, doctors, and others exposed to various forms of undue stress without adequate recovery.)
While increased workout volume (total time spent training) and exercise intensity (measured by heart rate) are often associated with OT, reduced recovery also plays a key role — even the best training schedule can impair the body when recovery is inadequate. A simple definition of successful exercise is an equation:
Training = Workout + Recovery
Training turns to OT as duration and/or intensity increases, and/or recovery is inadequate.
There is no single laboratory test to diagnose OT. Instead, athletes, coaches and clinicians rely on various physical, biochemical and mental-emotional indicators — clues in the form of signs and symptoms attributed to a single physiological factor: stress.
Referred to as a syndrome — a concurring set of related signs and symptoms associated with reduced health and fitness — the onset of OT can sometimes be elusive. Physiological adaptations to exercise vary considerably between individuals, therefore indications of OT can too. While images of a broken-down athlete are traditional, early stages of OT produce more modest but measurable impairment.
Functional overreaching is considered an optimal training state, preceding OT, with the advent of nonfunctional overreaching considered the onset of OT. (Due to autonomic imbalance associated with OT, the increased sympathetic activity sometimes leads to breakthrough or sudden great performance, however fleeting.)
Before discussing OT further, let’s put stress in perspective and consider how it can improve health and athletic performance.
Benefits of Exercise Stress
The body’s response to exercise — and in particular, the positive physical and biochemical stress it initiates — is the reason we benefit from it. Building a stronger, faster and more athletic body is due to adaptation to training stress, bringing untold health and fitness benefits. Gradually increasing exercise volume and intensity leads to more stress, which requires additional recovery, followed by more benefits.
The first response to training stress occurs in the brain through a complex neuroendocrine process of adaptation delivered to the body through nerves and hormones. It’s called the HPA (hypothalamic-pituitary-adrenal) axis, and is the same mechanism we use every day in adapting to other physical, biochemical and mental-emotional stressors. This process involves increases of two stress hormones, cortisol and epinephrine, including increased actions of the autonomic nervous system’s sympathetic and parasympathetic components.
- Physical stress includes those that affect the body’s structure, especially muscles and bones, and the equipment used, including footwear, involved in the physical workout, which affects posture and gait.
- The biochemical body generates energy from fat and sugar, manages hormones, and is strongly influenced by the quality of foods consumed.
- The mental-emotional aspect of training includes cognition, learning and the experience of it.
The healthy stress response to exercise can produce mild signs and symptoms such as some muscular fatigue, hunger and thirst, and a rewarding, euphoric response. However, undue stress can produce more muscle fatigue, weakness, soreness or pain, and stronger nutrient cravings. (While pain is not a normal feature of regular exercise, it often accompanies competition.)
Exercise benefits are directly related to physiological recovery from stress, also a function of the HPA axis. This requires varying amounts of time depending on the volume and intensity of exercise, and one’s health. Sleep quality and quantity is a key to effective recovery.
Other non-exercise stressors can also affect the process of adaptation. In particular, the kinds of foods consumed day-to-day play an important a role in training and recovery, as this significantly regulates conversion of stored fat and sugar to energy, and impacts the balance of inflammatory and anti-inflammatory chemicals. Social factors can produce stress as well, as can travel (circadian rhythm) and weather stress (especially temperature). Stress is cumulative, even in smaller amounts from these and other factors, increasing the need for additional recovery and adaptation.
One goal of exercise is to increase workout stress above a normal level to promote improved health and fitness that leads to better competitive performance; this state is referred to as functional overreaching.
Exceeding the body’s stress threshold, with excess training and/or reduced recovery (an imbalanced training equation) can induce excess exercise stress and maladaptation. The transition from functional to nonfunctional overreaching is described here as the onset of OT.
Three Stages of Overtraining
The spectrum of overtraining can be represented by three stages — the merging of a progressive, worsening state of health and fitness caused by the body’s inability to adapt to the accumulation of stress. These stressors may include:
- Increased exercise volume (daily or weekly hours).
- Increased high-intensity training (such as intervals, weight-lifting).
- Increased athletic competition.
- Reduced health (including allergies, asthma, hypertension, etc., or the need for over-the-counter or prescription medications).
- Poor diet (processed/junk food, inadequate calories, nutrient imbalance).
- Other non-exercise stress (personal, social).
- Inadequate recovery (especially poor sleep quality and quantity).
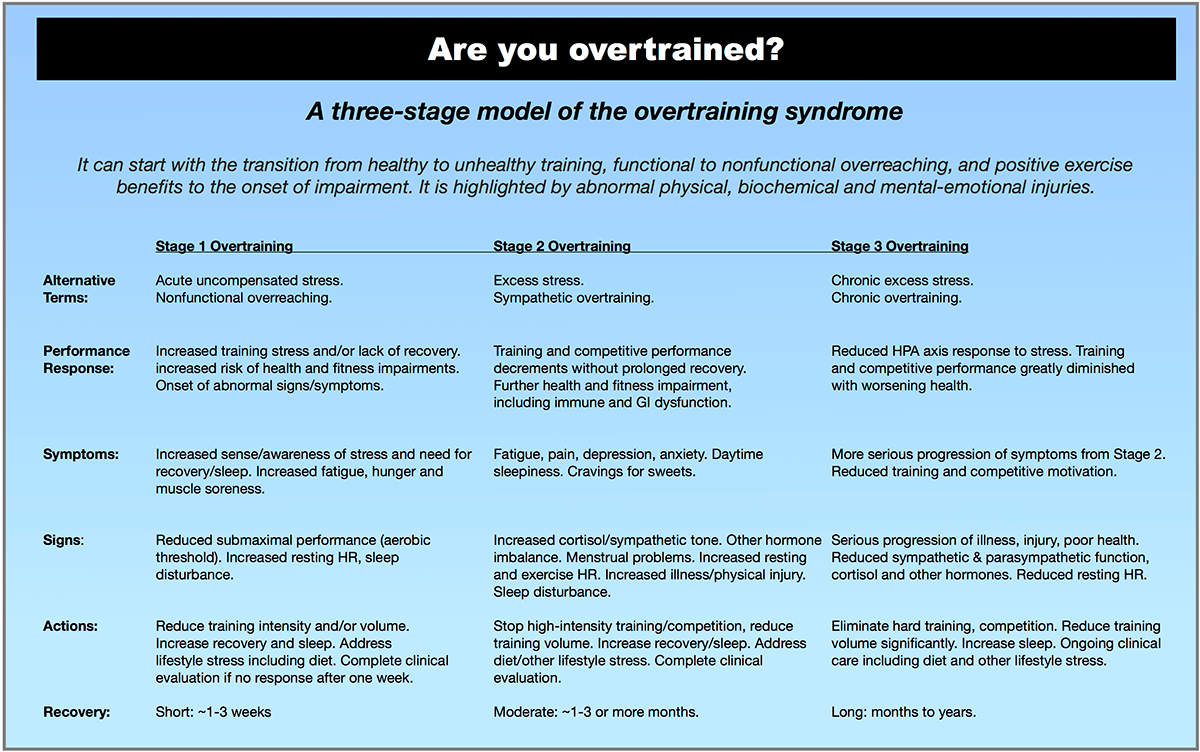
Stage 1 Overtraining
The transition from functional to nonfunctional overreaching can be considered the first stage of OT. While its recognition is not always obvious, identifying it presents the opportunity to prevent further serious physical, biochemical and mental-emotional problems, including injuries, and performance decrements.
Stage 1 OT is associated with the increased production of stress hormones and rise in sympathetic activity, with the onset of signs and symptoms:
- Athletes may become more aware of elevated stress, feel more fatigue/less energy during the day, with more physical soreness.
- Sleep quality or quantity may be affected, especially waking during the night unable to quickly return to sleep.
Monitoring the heart rate (HR) can be an important objective measure of OT. Increased sympathetic tone raises resting, submax and competitive HRs, reducing the aerobic threshold (also called FATmax, and MAF HR). As a result:
- Submax training HR, as measured using the MAF Test or GPS MAF Test, can increase; or may be indicated by reduced speed or power at the same previous HR.
- Resting HR can begin to elevate.
- Competitive HR can rise, reducing speed or power.
- Heart rate variability may demonstrate autonomic imbalance.
Interestingly, as mentioned previously, sometimes the increased sympathetic tone, a feature of functional overreaching, can continue and produce a sudden, often dramatic improvement in competitive performance, typically occurring only one time, after which impaired health and fitness becomes evident.
For the clinician, an impaired HPA axis becomes evident with the onset of elevated cortisol (tested through salivary cortisol) and chronic inflammation; excess sympathetic tone can promote intestinal disturbance and impaired immunity. In addition:
- Physical findings may include injuries to the low back, knee, ankle and foot.
- Biochemical impairment may produce fatigue, increased hunger or cravings for sweets or caffeine. Premenstrual or menopausal symptoms, and amenorrhea may be present in women; and sexual dysfunction may be apparent in men and women.
- Mental-emotional symptoms may include feelings of depression or anxiety.
Recovery from Stage 1 OT could be relatively fast and easy, with complete recovery and without detraining in one to three weeks if reductions of stress are obtained. Recommendations may include:
- Temporarily lowering training volume by 50-70 percent.
- Temporarily eliminating high-intensity training.
- Rest should include obtaining a minimum of 7-9 hours of uninterrupted sleep each night.
- Food habits include avoiding junk food (processed foods including sugar), and consuming adequate healthy fat and protein to meet caloric and other nutritional needs.
Normal training and competition can be gradually restored based on improved aerobic threshold as per the MAF Test, lowering of the resting HR (if previously elevated), and significant reductions of abnormal signs and symptoms. The process requires careful monitoring to prevent relapse, especially performing a monthly MAF Test and regular resting HR.
When early onset OT is not discovered or uncorrected, the physiologic changes can worsen merging into the second, more serious Stage 2.
Stage 2 Overtraining
Also called sympathetic overtraining, this stage is a deterioration of non-adapted stress that began in Stage 1. It is associated with specific neurological, hormonal and mechanical imbalances causing a variety of more obvious signs and symptoms.
Physical features may include:
- Resting, submax and maximal HRs are usually higher, leading to further deterioration of the aerobic threshold as indicated by the MAF Test (diminished speed and/or power at the same submax HR).
- Elevated competitive HR can diminish performances as well.
- Muscle imbalance (weakness and tightness of two or more muscles) can impair posture and gait, risking mechanical injuries to joints, bones and soft tissues, and promoting chronic physical soreness, fatigue and pain.
Biochemical indications may include:
- Immune dysfunction (increased colds, flu and other infections).
- Gut dysfunction (increased bloating, excess gas and intestinal discomfort, especially during training and competition).
- Reductions in FATmax leading to increasing or excess stored body fat, evaluated using the waist-to-height ratio (WtHR) .
Mental-emotional indications may include:
- Restlessness and over-excitability, especially in relation to reduced sleep.
- Increased potential for depression, anxiety.
- Increased general fatigue and daytime sleepiness.
A particular feature of Stage 2 OT is abnormally high cortisol, which can specifically lead to:
- Low testosterone in men and women (with subsequent muscle dysfunction and bone loss).
- Low thyroid hormone (thyroxin/T3), which may mimic hypothyroidism.
- Other hormone imbalances, reducing proper regulation of hydration and body temperature, and electrolytes, especially the excess loss of sodium.
- Increased insulin can further impair metabolism and increase body fat stores, especially in the abdomen and around the heart.
- Neurological performance may become impaired, including reduced sensory skills (keen awareness and fine hand-to-eye coordination) and reaction times required in many sports.
Health practitioners can play a key role in athlete care, especially during Stage 2 OT. A complete clinical evaluation is important, including history and physical examination, and appropriate laboratory testing. Dietary assessment is also very important to ensure a natural balanced diet is maintained, and ruling out disordered eating (which commonly accompanies OT).
The use of medication to treat secondary problems, such as poor sleep, depression or hormone imbalance, does not replace addressing the primary cause(s) of excess stress that may include training imbalance, poor diet and other lifestyle stress.
Recovery from Stage 2 OT may require one to three or more months, depending on the discipline of the athlete, although some require five to six months to improve FATmax and develop the aerobic system, a key part of recovery. In particular:
- All high-intensity training should be temporarily stopped, along with competition.
- Reduce training volume by 50-70 percent.
- An emphasis on more rest is vital, especially obtaining 7-9 or more hours of nightly uninterrupted sleep.
- Avoid junk food (processed foods including sugar).
- Consume adequate calories, including healthy fat and protein, to meet all nutritional needs.
Normal training and competition can be gradually restored once the aerobic threshold improves as per the MAF Test, resting HR returns to lower levels, laboratory tests normalize, and abnormal signs and symptoms, including any physical injuries, are eliminated. Ongoing monitoring to prevent relapse, especially performing a monthly MAF Test and resting HR, is important.
Many athletes remain in Stage 2 OT through a long vicious cycle of relapse and perceived recovery. Without correcting the primary causes of excess stress, some athletes can push themselves and progress to the third stage of OT.
Stage 3 Overtraining
A serious chronic excess stress condition, this end-stage of OT is associated with the exhaustion of neurological and hormonal mechanisms, typically with more severe physical, biochemical or mental-emotional consequences. Training and competitive performance continues worsening, with many athletes competing poorly or not at all.
Selye’s description of his Stage 3 was called a state of exhaustion, in part due to the condition of the adrenal glands, and is the inability of the HPA axis to compensate for the ongoing chronic excess stress. Adrenal exhaustion includes its failure to produce adequate cortisol and other vital hormones. Reduced sympathetic tone and overall autonomic function severely impairs metabolic and cardiovascular function (reflected in an abnormally low resting HR).
The lack of physical and mental energy reduces the desire to compete and sometimes train. Depression, significant physical injury, poor immunity and gut dysfunction are commonly associated with very poor health and fitness. There is an increased risk of hyponatremia — a serious, life-threatening condition of low blood sodium (which can begin in Stage 2) associated with reduced aldosterone — with the potential for water toxicity.
Recovery from Stage 3 OT, and return to previous optimal levels of performance is a very difficult task, and could take months to years. Athletes are seriously unwell, and require the help of healthcare practitioners to individualize appropriate treatments and monitoring.
- All moderate- to high-intensity and long workouts should be stopped, along with competition.
- Rest is vital, including as much uninterrupted nightly sleep as possible.
- Avoid junk food.
- Consume adequate healthy fat and protein in meeting all nutritional needs.
The three stages of OT are summarized in the following table:
Conclusion
Recognizing the overtraining syndrome in its earliest stage can help maximize human performance while remaining healthy. This process begins with a simple ongoing assessment process that evaluates physical, biochemical and mental-emotional signs and symptoms. The MAF Test may be an important tool for recognizing OT as a first objective sign, sometimes before the onset of symptoms. Restoring athletic performance to previous levels is most easily accomplished in Stage 1 OT, with Stage 2 requiring additional time and effort. Stage 3 OT is a more serious and difficult condition to address. Overall, prevention is the best remedy, allowing individuals to reach their athletic potential and maintain this state longer.