While the salt scare has all but ended, casualties remain. Some individuals with reduced health or genetic mutations may have elevated blood pressure when consuming levels of sodium that would otherwise be healthy for others.
Many people still believe that salt intake is the main culprit in high blood pressure, but even the American Heart Association has moved on from this myth.
Hypertension is a serious and dangerous condition of elevated blood pressure, and an indication that something is out of balance. One-third of the world’s population has high blood pressure, which is responsible for almost 50 percent of cardiovascular deaths. Normal pressure is considered less than 120 mmHg systolic and 80 mmHg diastolic (120/80); that level and above is abnormal. Prehypertension is considered 120-139/80-89, and hypertension above that level.
Elevated blood pressure is part of the chronic disease model, whereby excess body fat promotes chronic inflammation and carbohydrate intolerance, leading to poor health and fitness, including hypertension. In some cases, hypertension may be a side-effect of various drugs including NSAIDS (non-steroidal anti-inflammatory drugs), oral contraceptives, sympathicomimetics, anti-migraine and anti-dementia drugs, corticosteroids, antidepressants, antineuropathic, drugs for epilepsy, Parkinson’s disease, and others.
In most cases, improving lifestyle can reduce abnormally elevated blood pressure to normal without the need for medication — this is recommended as the first approach to treatment. Reducing excess body fat, typically caused by carbohydrate intolerance and corresponding elevations of insulin, often can bring desirable results relatively quickly, as this may be the most common cause of hypertension. This means eliminating all refined carbohydrate, especially sugar, from the diet.
During the Two-Week Test when carbohydrate intake is very low, elevated blood pressure may reduce rapidly, with those on medication potentially developing abnormally low blood pressure (hypotension), which can be dangerous. Asking your health practitioner to monitor your blood pressure during these lifestyle changes is important. In some people, blood pressure adaptation may take longer.
Just how long it takes for blood pressure to normalize, of course, depends on the individual. In short, those who become healthier and fitter sooner can reduce high blood pressure faster. In those with chronic inflammation, arterial stiffness — hardening of the arteries, or arteriosclerosis — often develops, which can make reductions in blood pressure a slower process, taking weeks, months, or longer (especially in those with diabetes or other diseases). Regular monitoring, especially when on medication, is essential.
Sodium Sensitivity
Most sodium consumed is sodium chloride found in various types of salt. While sodium is an important nutrient, one of the key electrolytes we all require, when the body’s hormones and other metabolic balance is off, too much sodium can raise blood pressure due to a condition called sodium sensitivity. But like other causes of hypertension, probably most cases can be remedied with a healthy lifestyle.
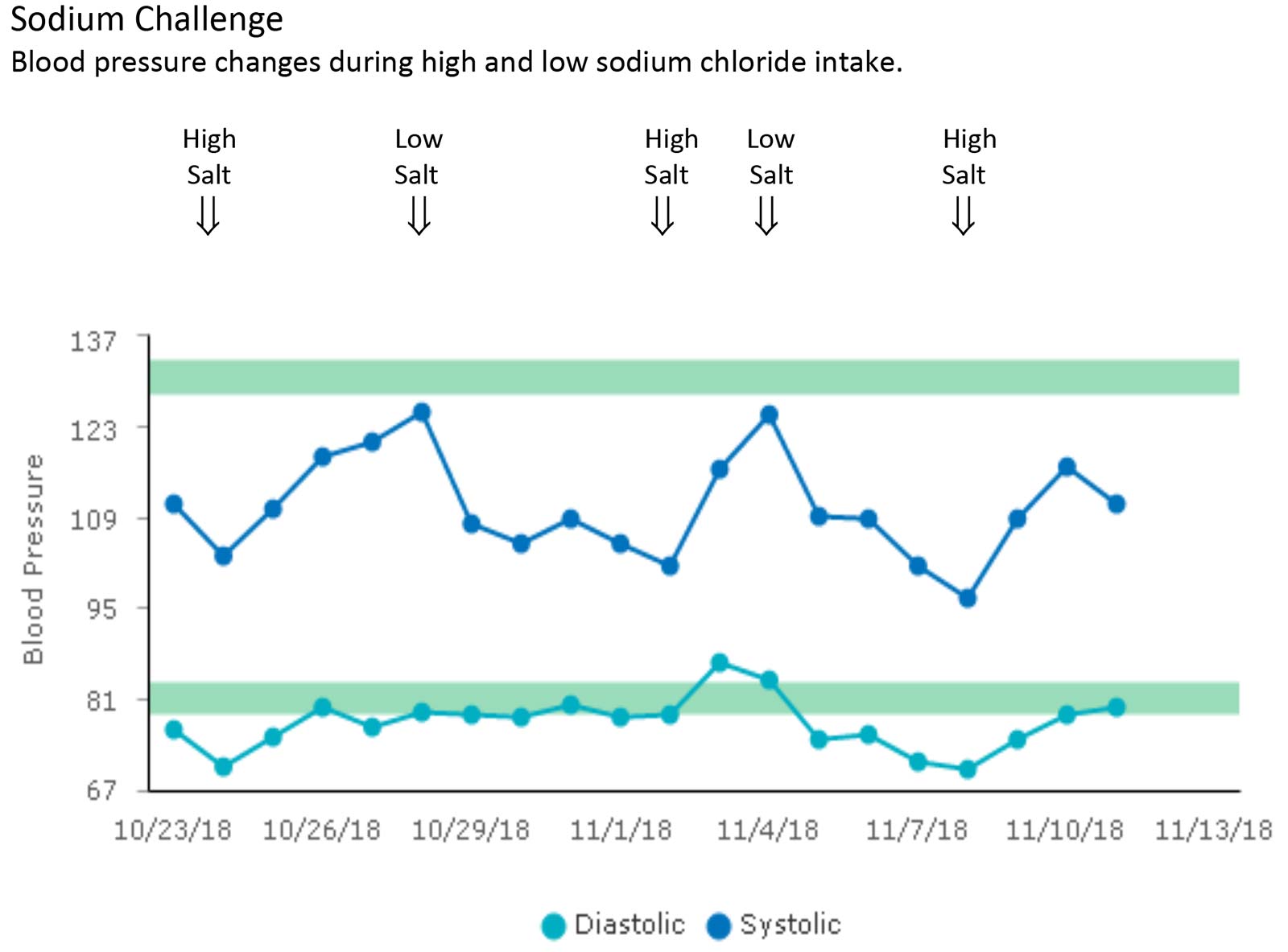
While those who have sodium sensitivity don’t usually feel it, this condition can sometimes manifest as slightly tight or swollen fingers after exercise, or excess water weight. There is no laboratory test for sodium sensitivity, but a dietary sodium challenge can help you discover if you’re sodium-sensitive. This would be indicated by a change in blood pressure of 5-10 percent (or at least 5mmHg) in response to a change in sodium chloride intake.
The chart below is an actual example of what can happen in a sodium-sensitive person during this challenge — blood pressure quickly trends downward when sodium is restricted from the diet, and rises when added back. During sodium restriction, the use of sodium chloride salt is avoided, along with high-sodium foods, which, in addition to most packaged and fast foods, includes smoked, cured, and salted meats and fish such as bacon and other sliced meats, and sardines, caviar and anchovies. The use of potassium chloride salt (also called salt substitute), which is low in sodium, is allowed in moderation.
Sodium sensitivity can develop for various reasons:
- Dysfunction of the sodium-regulatory mechanisms, particular in the kidneys, and the adrenal hormone aldosterone. This can be triggered by excess stress, raising the hormone cortisol.
- Excess body fat and associated chronic inflammation and carbohydrate intolerance (insulin resistance), which can create stress, and raise insulin, causing arterial stiffness, not allowing vessels to expand properly, raising blood pressure.
- A genetic mutation that can cause sodium sensitivity can adversely affect sodium metabolism and mechanisms affecting dilation of the arteries.
In addition, smaller numbers of people with normal blood pressure can be sodium-sensitive, a problem that can increase the risk for cardiovascular disease, asthma, osteoporosis, stomach cancer and kidney problems. Determining this sensitivity requires more complex assessments.
The recent recommendations by the Institute of Medicine for sodium chloride salt intake is up to 5.8 g (2.3 g, or 2300 mg, of sodium) for younger adults, a bit less for older adults. This is just over one teaspoon of salt daily. This amount of sodium would be too much for a person performing a sodium challenge.
Sodium Deficiency
Contrary to conventional wisdom, sodium deficiency is a frequent problem as well. It’s called hyponatremia, and is 10 times more common than heart attacks. In addition, writing in the journal Current Opinion in Nephrology and Hypertension (2013; Diagnostic tools for hypertension and salt sensitivity testing), Robin Felder and colleagues state that “a low-salt diet may not be beneficial to everyone and may paradoxically increase cardiovascular risk by raising blood pressure in some individuals.” This problem is called inverse salt sensitivity.
Athletes, and others who sweat a lot, may be more susceptible to increased sodium loss (sweat contains high amounts of sodium and little potassium). Increased high-intensity training can also cause excess sodium loss through the urine due to hormone imbalance.
Reducing blood pressure naturally by improving overall health can help other accompanying health issues, and is the first line of treatment. This is directed at reducing and maintaining body fat to normal levels, which reduces carbohydrate intolerance and insulin, something most easily accomplished by avoiding junk food, especially sugar and other refined carbohydrates. Improving health to lower blood pressure is usually effective enough to avoid or eliminate medication. In some cases, this may mean reducing sodium intake to levels that don’t raise blood pressure (see chart).
Once again, for those already on prescription drugs for high blood pressure, getting your health practitioner’s help is important for careful monitoring and reducing or eliminating medication as needed. This is important, as better eating can reduce blood pressure, and medication continues doing the same. Lowering blood pressure too much with medication is dangerous; it can impair health, especially for the brain.
Studies have demonstrated the benefits of improved lifestyle for optimal health and fitness, and addressing hypertension is no exception. In difficult cases, sodium sensitivity should also be considered.